

Indian Journal of Science and Technology
DOI: 10.17485/IJST/v15i17.2330
Year: 2022, Volume: 15, Issue: 17, Pages: 806-810
Original Article
C R Raghavendra1*, G Yuvabalakumaran2, Reena Rajan3, R M Sidhesh4, S Mathavi5
1Junior Resident, Department of Radiology, Vinayaka Mission Kirupananda Variyar Salem, Tamil Nadu, India
2Associate Professor, Department of Radiology, Vinayaka Mission Kirupananda Variyar Salem, Tamil Nadu, India
3Assistant professor, Department of Microbiology, Vinayaka Mission Kirupananda Variyar Salem, Tamil Nadu, India
4Assistant professor. Department of Radiology, Vinayaka Mission Kirupananda Variyar Salem, Tamil Nadu, India
5Proffesor and Head of department, Department of Microbiology, Vinayaka Mission Kirupananda Variyar Salem, Tamil Nadu, India
*Corresponding Author
Email: [email protected]
Received Date:31 December 2021, Accepted Date:13 March 2022, Published Date:12 May 2022
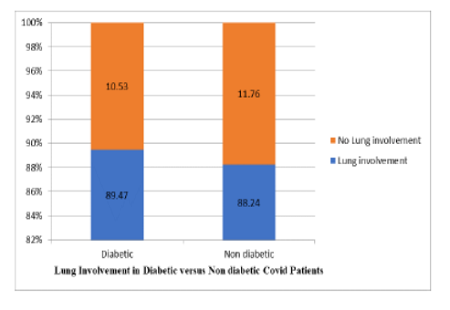
Background/Objectives: The Corona virus disease 2019 (Covid 19) pandemic has emerged as a great challenge to healthcare system with high rate of hospitalization and deaths. People with co morbidities such as diabetes are at increased risk of complications and Covid 19 associated deaths. The present study was done to evaluate Covid 19 severity among diabetic and nondiabetic patients using Chest CT severity score. Methods: A total of 106 Patients were subjected to standardized High Resolution Computed Tomography (HRCT) chest imaging. The analyzed images and Computed Tomography (CT) severity score was grouped into mild, moderate, severe and no lung involvement in both diabetic and nondiabetic group. Findings: Among the diabetic patients 39.47% showed CT severity score of 15-25 compared to 8.82% in nondiabetic patients. Lung involvement was observed in 89.47% diabetic compared to 88.24% nondiabetic patients. Novelty: Diffuse ground glass opacity involving all the lobes was observed among poorly controlled diabetic patients whereas patch ground glass opacity was observed among nondiabetic group. By chest CT severity scoring, the severity of lung involvement due to Covid 19 in Diabetes mellitus patients was found to be greater (39.47%) when compared to nondiabetic individual (8.82%).
Keywords: Computed Tomography chest imaging; Computed Tomography severity score; Diabetes mellitus; Lung involvement; Covid 19 severity
© 2022 Raghavendra et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By Indian Society for Education and Environment (iSee)
Subscribe now for latest articles and news.