

Indian Journal of Science and Technology
Year: 2020, Volume: 13, Issue: 19, Pages: 1908-1916
Original Article
Nohra Diaz-Cornejo1 , Luis Ruiz-Garcés1∗, José Ortiz-Girón1 , Nathalie RamirezBarbera1
1 Faculty of Health Science, University of Sinu, Medicine Program, Monteria, Colombia
∗Corresponding author:
Luis Ruiz-Garcés
Faculty of Health Science, University of Sinu, Medicine Program, Monteria, Colombia
Email: [email protected]
Received Date:19 April 2020, Accepted Date:01 May 2020, Published Date:18 June 2020
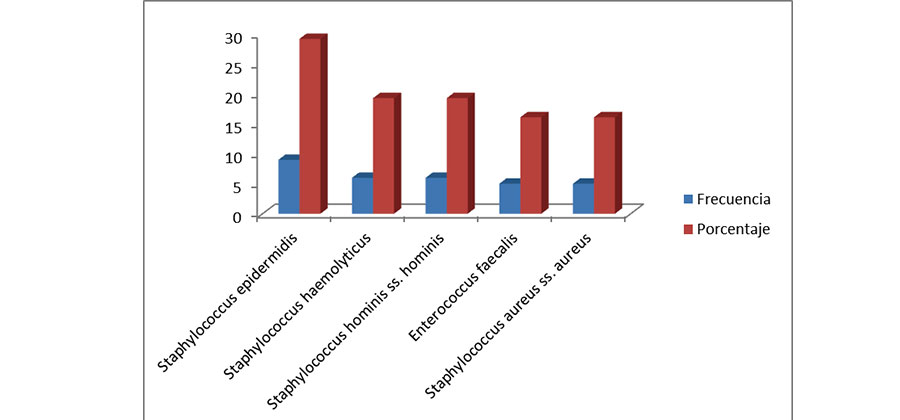
Objectives: To determine the most frequent bacterial pathogens in the bloodstream and their resistance profiles in a hospital institution in Monteria - Cordoba. Methods: An observational study was conducted, during the months of January to December 2018, 113 blood samples from patients with sepsis were evaluated. The identification and susceptibility of the bacteria were determined through the VITEK system, using the GNI + cards for Gram-negative bacilli and GPI for Gram-positive cocci and the GNS 113 and GPS 102 cards for Gram-negative bacilli and Gram-positive cocci respectively. Findings: Among the Gram-negative bacteria, the ones that were most frequently isolated were Pseudomonas aeruginosa, Klebsiella pneumonia and Acinetobacter baumannii; while among the Gram-positive bacteria Staphylococcus epidermidis was the pathogen that was most frequently isolated. Gram-negative Pseudomonas aeruginosa isolates showed high resistance to doripenem, imipenem and meropenem. Acinetobacter baumannii showed high resistance to most antibiotics. Serratia marcescens, Escherichia coli, Enterobacter cloacae had a low resistance rate. Gram-positive Staphylococcus epidermidis, Staphylococcus haemolyticus, Staphylococcus hominis ss. hominis, Enterococcus faecalis and Staphylococcus aureus ss. aureus showed high resistance to erythromycin. Novelty: A high prevalence of antimicrobial resistance was observed in the present investigation.
Keywords: Blood culture; bacteremia; antimicrobial resistance; sepsis
© 2020 Diaz-Cornejo, Ruiz-Garcés, Ortiz-Girón, Ramirez-Barbera. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Published By Indian Society for Education and Environment (iSee)
Subscribe now for latest articles and news.