

Indian Journal of Science and Technology
DOI: 10.17485/IJST/v14i20.2011
Year: 2021, Volume: 14, Issue: 20, Pages: 1689-1698
Original Article
S T Veerabhadrappa✉ 1 , P M Shivakumara Swamy 1 , G C Suguna 1 , S K Srinidhi 1 , D Priyanka 1
1Department of Electronics and Communication Engineering, JSS Academy of Technical Education, Bengaluru, 560060, India
Received Date:05 November 2020, Accepted Date:26 April 2021, Published Date:08 June 2021
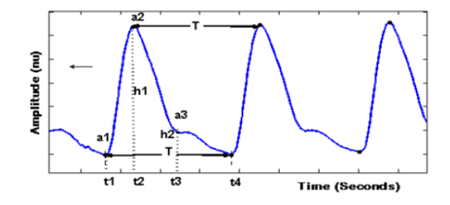
Objectives: To develop a non-invasive measurement of continuous monitoring of hemoglobin using IoT-enabled pulse oximetry. Currently in India, most women, senior citizens, and rural area people are suffering from anemia. In many cases, people unable to visit hospitals and laboratories for hemoglobin testing. To help the above people our proposed system will measure hemoglobin concentration without visiting the hospital at an affordable price. Methods: We developed real-time continuous monitoring of Hb concentration and oxygen saturation (SpO2) using pulse oximetry. In this study, 47 healthy volunteers were participated and measure the above-mentioned parameters under resting conditions. Findings: The obtained results were in unison with laboratory measurements with the variation of 0.12g/dL to 1.0g/dL. Novelty/Applications: Experimental results showed the approach of continuous monitoring of hemoglobin and SpO2 using an IoT-enabled non-invasive method can be useful in healthcare management.
Keywords
Hemoglobin, oxygen saturation, pulse oximetry, IoT, Anaemia
© 2021 Veerabhadrappa et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Published By Indian Society for Education and Environment (iSee)
Subscribe now for latest articles and news.